Recipe for Health
By Steve Hendershot
UIC researchers and health care providers partner with communities to address underlying causes of health disparities
Video: Anthony Jackson
“Who can tell me about egg grading?” That might sound like a question for culinary students, but instead, it’s posed to a group of women with hypertension, or high blood pressure. The condition stems partly from a diet that’s too high in salt, and the women are gathered in the basement of a church in Chicago’s South Shore neighborhood to learn new cooking methods from Chef Ken L. Polk.
Polk ticks through the differences between eggs rated AA, A and B, and the appropriate uses for each. (Grade AA eggs generally are reserved for restaurants because they’re best for presentation, while if you’re forced to use Grade B eggs, it’s best to scramble them rather than cook them over-easy.)
While the women are learning new knife skills, ingredients and flavor combinations, Polk’s intent isn’t to vault them onto the next season of Top Chef. Rather, it’s to share ways to cook healthier, low-sodium meals.
“They learn how to switch up spices to get more flavor, whereas salt is just one particular seasoning in the arsenal,” says Polk. In every recipe he presents, “salt is the last ingredient, so they can ascertain whether they can add it.”
The class is the brainchild of Saria Lofton, assistant professor at the University of Illinois Chicago’s College of Nursing, who studies the prevalence of hypertension among Black women.
According to the U.S. Centers for Disease Control and Prevention, Black women are 50% more likely than white women to have high blood pressure, and Black people overall are 30% more likely than white people to die from heart disease — the leading cause of death in America.
Those hypertension disparities contribute to a broader, more concerning gap in health outcomes. The life expectancy for Black people is nearly five years shorter than for white people, according to a new study from the Kaiser Family Foundation.
The divergence in outcomes points to a growing field of study around the cultural and environmental factors influencing people’s health. Lofton and other researchers at UIC and UI Health, the university’s academic health enterprise, want to better understand the correlations and to intervene with services that can bridge the divide.
Through the classes, Lofton, Polk and community health advocate Amena Karim aim to support participants who want to eat and live more healthfully. Flavor — for flavor’s sake, anyway — isn’t exactly the point. Instead, the class is first an act of health care.
One participant, Katrina Gatson, earned rave reviews from her family after introducing new ingredients and techniques, from cumin to asparagus to stir-fry. Salt, formerly a go-to source of seasoning, has all but disappeared from her family’s table.
The cooking class is one of many UIC initiatives to understand health disparities and improve outcomes for people in communities with high rates of disease and chronic health conditions. Researchers are examining cultural and environmental factors ranging from access to healthy food to how people from different backgrounds engage with and experience the health care system.
Their findings lead to solutions that sometimes go beyond the traditional boundaries of health care. The cooking class is one example. Another is the Health in All Policies Workgroup, a partnership between UIC’s School of Public Health (SPH) and the Illinois Department of Public Health that examines proposed legislation related to topics such as housing and education through a public health lens.
The focus on the health implications of social factors is a relatively recent phenomenon, says Dr. Wayne Giles, dean of SPH and co-chair of the Health in All Policies Workgroup.
The initiatives speak to a growing recognition that bridging gaps in health outcomes will require innovation, collaboration and flexibility beyond the traditional scope of health care.
Improving health outcomes for people in high-risk groups requires a multipronged strategy, says Giles.
Health providers can still “address proximal issues like access to care, immunizations or providing people with medication for conditions like hypertension. But as you’re providing those things, you also want to provide safe places to be physically active and opportunities to eat healthy foods, and make sure you’re focused on issues like housing and education.”
Outcome Influencers: Housing and Trauma
Photo: Anthony Jackson
Last year, the Health in All Policies Workgroup looked at housing, recommending that the state appropriate funds to transition unhoused people into supportive housing, which is a crucial underlying issue for people’s health.
“It’s hard for people to concentrate on being and staying healthy and taking their medication when they’re focused on finding a safe place to sleep at night,” Giles says.
That insight squares with the work of Stephen Brown, director of preventive emergency medicine within UI Health’s Department of Emergency Medicine.
Brown studies unhoused people’s health care usage patterns, including use of emergency departments for regular or preventive care. That trend, combined with high rates of severe and persistent mental illness within the unhoused population, is a recipe for bad outcomes.
In response, Brown helps run a UI Health-funded program that offers housing as part of its care plan. More than 120 individuals and families have gained housing through the program since its inception in 2017, and Brown says it’s the longest-running program in the country.
Often there are irrevocable health effects on people who have lived without housing for an extended period, and the focus of care providers “is on getting them stable,” says Brown, who is also director of business development within the Institute for Healthcare Delivery Design.
Similarly, people who have experienced substantial emotional trauma also are at greater risk of health problems.
Trauma-related disorders arise “when we have too many bad experiences, and not enough good experiences, and our brain and body’s usual regulation mechanisms get disrupted,” says Audrey Stillerman, a clinical associate professor within UIC’s Department of Family and Community Medicine in the College of Medicine.
“If we don’t have time to recover, we get stuck on high alert,” Stillerman says.
Repeated exposure to traumatic events can disrupt the body’s physiologic systems and contribute to the onset of multiple physical and mental health conditions such as diabetes, depression and substance use, adds Stillerman, who is also medical director for Mile Square’s school health center program, which includes four of the 11 clinics in the UI Health Mile Square enterprise, which provides high-quality health services to underserved communities.
Perhaps it’s no surprise, then, that one of the women attending the cooking classes at the South Shore church brings along two kids who were recently exposed to gun violence.
The program’s organizers, Lofton and Karim, both subscribe to the mantra “food is medicine,” and hope that the warm community assembled in the church kitchen will bring emotional healing and nutritional wisdom.
Bringing the system to the people — and vice versa
Photo courtesy of UI Health.
UIC’s downtown medical campus and the surrounding Illinois Medical District offer a powerful concentration of health care resources. Yet for some people, the campus — and the health system more broadly — feel intimidating and unapproachable.
“It’s scary to go to the big campus” for some people unfamiliar with the health system, says Silvia Lara, family nurse practitioner at Davis Health and Wellness Center, a school-based health center that’s part of UI Health Mile Square Health Center.
For large health systems across the country, capacity often outpaces connection. That contributes to a gap in access to care. One scoring system from Commonwealth Fund, a New York City-based foundation, rates access to care for white Illinois residents at 82 out of 100, compared to 42 for Hispanic residents and 17 for Black residents.
A lack of confidence in navigating the health system is one contributing factor; others are a relative dearth of community-based health care options in economically disadvantaged areas, as well as transportation costs connected to getting to and from health care hubs.
While health disparities often are framed through a race- or gender-based lens, “a lot of these health-related social needs are really rooted in income,” notes Rani Williams, chief diversity and community health equity officer at UI Health.
Community-based efforts have additional benefits, too, such as the on-the-ground insight gained by providers, as well as those gathered by community health workers — professionals whose job is to visit neighborhood residents and function as a conduit between the health care system and people who struggle with access.
One example comes from Victoria Persky, a UIC professor of epidemiology and biostatistics who spent decades studying race-based gaps in asthma prevalence and asthma-related deaths, and who now is researching health issues related to metal exposure. In addition to her research, Persky also helped found Mobile Care Chicago, a service that provides on-site asthma care to children in disadvantaged communities.
A family connected to one of Persky’s studies couldn’t seem to alleviate their child’s asthma, despite employing all the suggested remedies. A community health worker from one of Persky’s studies doing a home evaluation found a large number of birds that may have been exacerbating the child’s asthma, a finding that had not been noted by the child’s medical provider. Removing some of the birds and cleaning the home was a straightforward fix — but one that the care team wouldn’t have identified without a community presence.
Another example comes from one of the school-based community health centers run by UI Health Mile Square Health Center. Leaders at the Davis Health and Wellness Center, located within Nathan S. Davis Elementary School, in Chicago’s southwest side Brighton Park neighborhood, didn’t initially realize that hunger was a major issue for families in the community.
“In the Latino community, many times we don’t talk about our needs; we just give a good presentation,” says Jose Lopez, a community health worker who helps coordinate the monthly events. “It’s ‘Everything is great!’ in your house — but in reality, there’s no food; you have problems.”
The clinic’s community presence fostered a great level of connection and observation, however, and one of the nurses began bringing food that she collected from church. That got the attention of the clinic’s leaders and led to a formal partnership with the Greater Chicago Food Depository — and a recurring food pantry that now draws more than 100 families each month.
It’s one reason the community-based Mile Square Health Center clinics are essential to UI Health’s mission. But UI Health leaders also are working to make every element of the system more accessible.
In some cases, the challenges stem from the complicated structure of the American health system. In other instances, the roadblocks are sometimes cultural, such as when Spanish-speaking patients struggle to communicate with English-speaking care providers; or logistical, when job- or transportation-related issues make it difficult for people to see providers.
Identifying and addressing those pain points is part of the impetus behind UIC’s Institute for Healthcare Delivery Design (IHDD), which attempts to analyze the health care system using a consumer experience-focused methodology similar to that used in product and service design. Its goal is to design improvements that better serve patients while accommodating the many constraints of care delivery in a highly regulated industry with complex insurance requirements and expansive data privacy laws.
“These are very complex problems, and design is frequently brought in to address what are described as wicked problems — things that don’t lend themselves to easy solutions,” says Hugh Musick, assistant vice chancellor of population health sciences at UIC and co-director of IHDD.
IHDD began in 2017 and quickly partnered with Illinois state government leaders to investigate ways to improve the care delivered through the state’s Medicaid system. The insights gleaned through interviews with Medicaid patients helped inform a 2021 state law that allocated new funding to support health care transformation collaboratives—creative partnerships between health systems and community partners.
Theresa Eagleson, then-director of the Illinois Department of Healthcare and Family Services, describes the approach as “venture capital for Medicaid providers — because that’s not an opportunity that providers serving poor people often get, to try to figure out a better way to serve people in their communities.” (Eagleson left state government last year after a three-decade career and joined IHDD.)
The 2021 act led to the creation of more than a dozen collaboratives across the state, including a specialty-care clinic in Chicago’s Gage Park that includes contributions from UIC and UI Health and community partners such as Alivio Medical Center and Friend Family Health Center.
The Institute’s research showed that having to travel more than a couple miles to a health care facility is a meaningful barrier to care. By bringing specialty care to where people live enables the clinic “to be viewed as a part of the community,” Musick says.
Health campuses also are working to become more user-friendly to the access-challenged. Last fall, UI Health launched a pilot program providing free transportation to and from its Taylor Street campus for patients who meet certain criteria such as income level and not having insurance-based transportation benefits.

The sky bridge connecting University of Illinois Hospital & Health Sciences System buildings. Photo courtesy of UI Health.
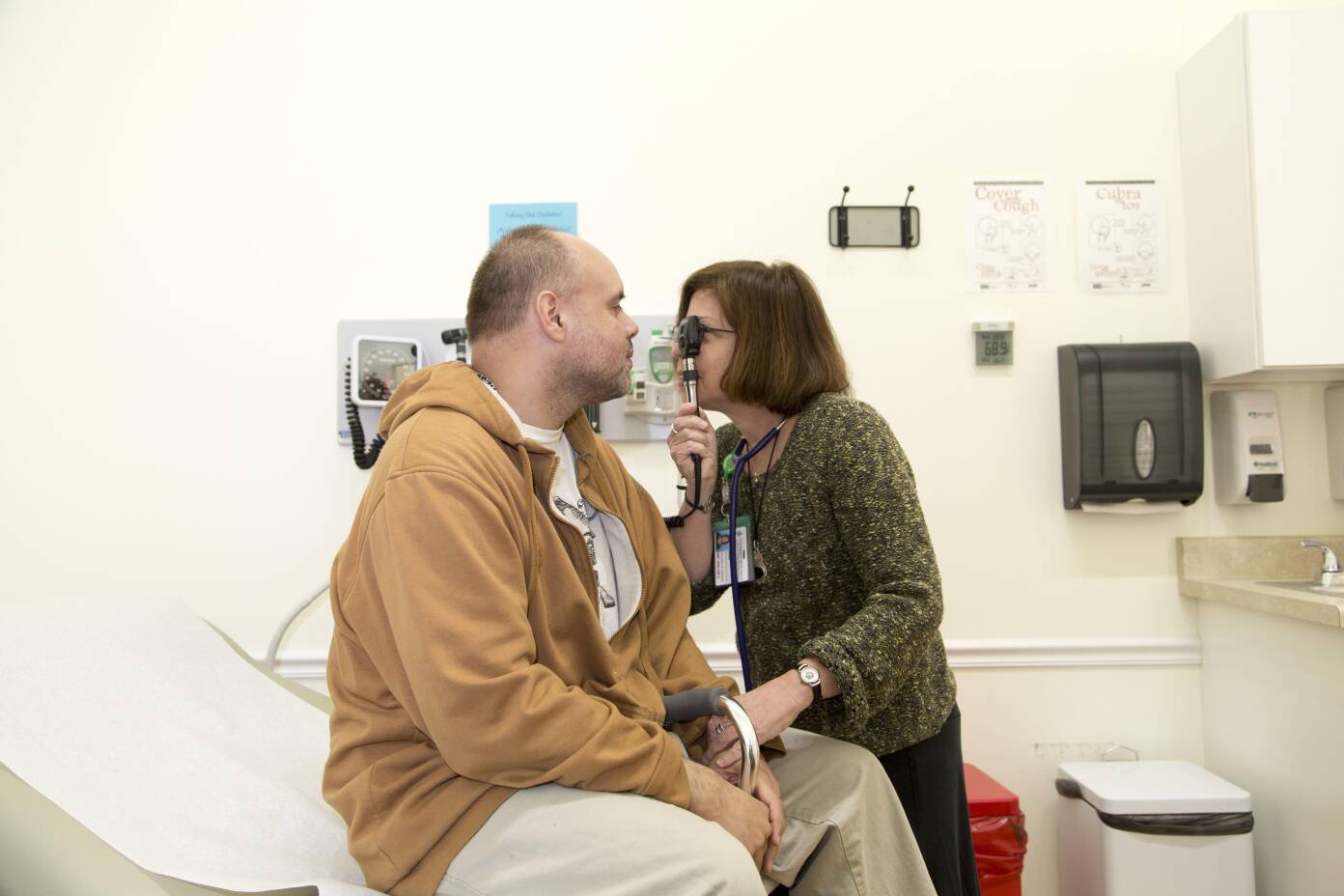
A patient receives a health examination at Humboldt Park's Mile Square Health Center. Photo courtesy of UI Health.
Making it easier to be healthy
Photo: Anthony Jackson

For all the complex factors that influence health outcomes — from genetics to behaviors, cultural factors, life experiences and medicine — a nutritious diet is among the most important. For health professionals, encouraging people to eat healthfully means making it easy to cook and eat well.
So when Chef Polk leads the South Shore cooking classes, he recommends widely available ingredients that participants can get without traveling too far. Lofton, the UIC researcher behind the program, is mindful of participants who rely on public transportation or ride-shares to get to stores that, in disadvantaged areas, are often located far from home.
For people who don’t have access to nearby parks or who don’t feel safe outdoors, another staple of preventive health care — exercise — can be similarly challenging.
Those are the situations that get high-level systems designers such as the Institute for Healthcare Delivery and Design’s Musick to think about community- or policy-level interventions, while on-the-ground practitioners such as Silvia Lara from the Davis Health and Wellness Center focus on devising workarounds such as YouTube workouts and at-home push-up regimens.
Yet beyond administering care and sharing best practices, among the most powerful gifts a provider can offer to a patient are hope and confidence.
These days, cooking-class participant Katrina Gatson is feeling both as she’s grown passionate about cooking healthfully for herself and her family.
She’s got a piece of advice for would-be chefs that could also serve as a prescription for a country and health system looking to improve the care it delivers: “Try new things,” Gatson says. “Don’t be afraid. Just because you tried something one way doesn’t mean you couldn’t try it a different way and like it even better.”
Video: Anthony Jackson
Recipe
for
Health
By Steve Hendershot
UIC researchers and health care providers partner with communities to address underlying causes of health disparities
“Who can tell me about egg grading?” That might sound like a question for culinary students, but instead, it’s posed to a group of women with hypertension, or high blood pressure. The condition stems partly from a diet that’s too high in salt, and the women are gathered in the basement of a church in Chicago’s South Shore neighborhood to learn new cooking methods from Chef Ken L. Polk.
Polk ticks through the differences between eggs rated AA, A and B, and the appropriate uses for each. (Grade AA eggs generally are reserved for restaurants because they’re best for presentation, while if you’re forced to use Grade B eggs, it’s best to scramble them rather than cook them over-easy.)
While the women are learning new knife skills, ingredients and flavor combinations, Polk’s intent isn’t to vault them onto the next season of Top Chef. Rather, it’s to share ways to cook healthier, low-sodium meals.
“They learn how to switch up spices to get more flavor, whereas salt is just one particular seasoning in the arsenal,” says Polk. In every recipe he presents, “salt is the last ingredient, so they can ascertain whether they can add it.”
The class is the brainchild of Saria Lofton, assistant professor at the University of Illinois Chicago’s College of Nursing, who studies the prevalence of hypertension among Black women.
According to the U.S. Centers for Disease Control and Prevention, Black women are 50% more likely than white women to have high blood pressure, and Black people overall are 30% more likely than white people to die from heart disease — the leading cause of death in America.
Those hypertension disparities contribute to a broader, more concerning gap in health outcomes. The life expectancy for Black people is nearly five years shorter than for white people, according to a new study from the Kaiser Family Foundation.
The divergence in outcomes points to a growing field of study around the cultural and environmental factors influencing people’s health. Lofton and other researchers at UIC and UI Health, the university’s academic health enterprise, want to better understand the correlations and to intervene with services that can bridge the divide.
Through the classes, Lofton, Polk and community health advocate Amena Karim aim to support participants who want to eat and live more healthfully. Flavor — for flavor’s sake, anyway — isn’t exactly the point. Instead, the class is first an act of health care.
One participant, Katrina Gatson, earned rave reviews from her family after introducing new ingredients and techniques, from cumin to asparagus to stir-fry. Salt, formerly a go-to source of seasoning, has all but disappeared from her family’s table.
The cooking class is one of many UIC initiatives to understand health disparities and improve outcomes for people in communities with high rates of disease and chronic health conditions. Researchers are examining cultural and environmental factors ranging from access to healthy food to how people from different backgrounds engage with and experience the health care system.
Their findings lead to solutions that sometimes go beyond the traditional boundaries of health care. The cooking class is one example. Another is the Health in All Policies Workgroup, a partnership between UIC’s School of Public Health (SPH) and the Illinois Department of Public Health that examines proposed legislation related to topics such as housing and education through a public health lens.
The focus on the health implications of social factors is a relatively recent phenomenon, says Dr. Wayne Giles, dean of SPH and co-chair of the Health in All Policies Workgroup.
The initiatives speak to a growing recognition that bridging gaps in health outcomes will require innovation, collaboration and flexibility beyond the traditional scope of health care.
Improving health outcomes for people in high-risk groups requires a multipronged strategy, says Giles.
Health providers can still “address proximal issues like access to care, immunizations or providing people with medication for conditions like hypertension. But as you’re providing those things, you also want to provide safe places to be physically active and opportunities to eat healthy foods, and make sure you’re focused on issues like housing and education.”
Outcome Influencers: Housing and Trauma
Photo: Anthony Jackson
Last year, the Health in All Policies Workgroup looked at housing, recommending that the state appropriate funds to transition unhoused people into supportive housing, which is a crucial underlying issue for people’s health.
“It’s hard for people to concentrate on being and staying healthy and taking their medication when they’re focused on finding a safe place to sleep at night,” Giles says.
That insight squares with the work of Stephen Brown, director of preventive emergency medicine within UI Health’s Department of Emergency Medicine.
Brown studies unhoused people’s health care usage patterns, including use of emergency departments for regular or preventive care. That trend, combined with high rates of severe and persistent mental illness within the unhoused population, is a recipe for bad outcomes.
In response, Brown helps run a UI Health-funded program that offers housing as part of its care plan. More than 120 individuals and families have gained housing through the program since its inception in 2017, and Brown says it’s the longest-running program in the country.
Often there are irrevocable health effects on people who have lived without housing for an extended period, and the focus of care providers “is on getting them stable,” says Brown, who is also director of business development within the Institute for Healthcare Delivery Design.
Similarly, people who have experienced substantial emotional trauma also are at greater risk of health problems.
Trauma-related disorders arise “when we have too many bad experiences, and not enough good experiences, and our brain and body’s usual regulation mechanisms get disrupted,” says Audrey Stillerman, a clinical associate professor within UIC’s Department of Family and Community Medicine in the College of Medicine.
“If we don’t have time to recover, we get stuck on high alert,” Stillerman says.
Repeated exposure to traumatic events can disrupt the body’s physiologic systems and contribute to the onset of multiple physical and mental health conditions such as diabetes, depression and substance use, adds Stillerman, who is also medical director for Mile Square’s school health center program, which includes four of the 11 clinics in the UI Health Mile Square enterprise, which provides high-quality health services to underserved communities.
Perhaps it’s no surprise, then, that one of the women attending the cooking classes at the South Shore church brings along two kids who were recently exposed to gun violence.
The program’s organizers, Lofton and Karim, both subscribe to the mantra “food is medicine,” and hope that the warm community assembled in the church kitchen will bring emotional healing and nutritional wisdom.
Photo courtesy of UI Health.
Bringing the system to the people — and vice versa
Community-based efforts have additional benefits, too, such as the on-the-ground insight gained by providers, as well as those gathered by community health workers — professionals whose job is to visit neighborhood residents and function as a conduit between the health care system and people who struggle with access.
One example comes from Victoria Persky, a UIC professor of epidemiology and biostatistics who spent decades studying race-based gaps in asthma prevalence and asthma-related deaths, and who now is researching health issues related to metal exposure. In addition to her research, Persky also helped found Mobile Care Chicago, a service that provides on-site asthma care to children in disadvantaged communities.
A family connected to one of Persky’s studies couldn’t seem to alleviate their child’s asthma, despite employing all the suggested remedies. A community health worker from one of Persky’s studies doing a home evaluation found a large number of birds that may have been exacerbating the child’s asthma, a finding that had not been noted by the child’s medical provider. Removing some of the birds and cleaning the home was a straightforward fix — but one that the care team wouldn’t have identified without a community presence.
Another example comes from one of the school-based community health centers run by UI Health Mile Square Health Center. Leaders at the Davis Health and Wellness Center, located within Nathan S. Davis Elementary School, in Chicago’s southwest side Brighton Park neighborhood, didn’t initially realize that hunger was a major issue for families in the community.
“In the Latino community, many times we don’t talk about our needs; we just give a good presentation,” says Jose Lopez, a community health worker who helps coordinate the monthly events. “It’s ‘Everything is great!’ in your house — but in reality, there’s no food; you have problems.”
The clinic’s community presence fostered a great level of connection and observation, however, and one of the nurses began bringing food that she collected from church. That got the attention of the clinic’s leaders and led to a formal partnership with the Greater Chicago Food Depository — and a recurring food pantry that now draws more than 100 families each month.

The sky bridge connecting University of Illinois Hospital & Health Sciences System buildings. Photo courtesy of UI Health.
It’s one reason the community-based Mile Square Health Center clinics are essential to UI Health’s mission. But UI Health leaders also are working to make every element of the system more accessible.
In some cases, the challenges stem from the complicated structure of the American health system. In other instances, the roadblocks are sometimes cultural, such as when Spanish-speaking patients struggle to communicate with English-speaking care providers; or logistical, when job- or transportation-related issues make it difficult for people to see providers.
Identifying and addressing those pain points is part of the impetus behind UIC’s Institute for Healthcare Delivery Design (IHDD), which attempts to analyze the health care system using a consumer experience-focused methodology similar to that used in product and service design. Its goal is to design improvements that better serve patients while accommodating the many constraints of care delivery in a highly regulated industry with complex insurance requirements and expansive data privacy laws.
“These are very complex problems, and design is frequently brought in to address what are described as wicked problems — things that don’t lend themselves to easy solutions,” says Hugh Musick, assistant vice chancellor of population health sciences at UIC and co-director of IHDD.
IHDD began in 2017 and quickly partnered with Illinois state government leaders to investigate ways to improve the care delivered through the state’s Medicaid system. The insights gleaned through interviews with Medicaid patients helped inform a 2021 state law that allocated new funding to support health care transformation collaboratives—creative partnerships between health systems and community partners.
Theresa Eagleson, then-director of the Illinois Department of Healthcare and Family Services, describes the approach as “venture capital for Medicaid providers — because that’s not an opportunity that providers serving poor people often get, to try to figure out a better way to serve people in their communities.” (Eagleson left state government last year after a three-decade career and joined IHDD.)
The 2021 act led to the creation of more than a dozen collaboratives across the state, including a specialty-care clinic in Chicago’s Gage Park that includes contributions from UIC and UI Health and community partners such as Alivio Medical Center and Friend Family Health Center.
The Institute’s research showed that having to travel more than a couple miles to a health care facility is a meaningful barrier to care. By bringing specialty care to where people live enables the clinic “to be viewed as a part of the community,” Musick says.
Health campuses also are working to become more user-friendly to the access-challenged. Last fall, UI Health launched a pilot program providing free transportation to and from its Taylor Street campus for patients who meet certain criteria such as income level and not having insurance-based transportation benefits.

A patient receives a health examination at Humboldt Park's Mile Square Health Center. Photo courtesy of UI Health.
UIC’s downtown medical campus and the surrounding Illinois Medical District offer a powerful concentration of health care resources. Yet for some people, the campus — and the health system more broadly — feel intimidating and unapproachable.
“It’s scary to go to the big campus” for some people unfamiliar with the health system, says Silvia Lara, family nurse practitioner at Davis Health and Wellness Center, a school-based health center that’s part of UI Health Mile Square Health Center.
For large health systems across the country, capacity often outpaces connection. That contributes to a gap in access to care. One scoring system from Commonwealth Fund, a New York City-based foundation, rates access to care for white Illinois residents at 82 out of 100, compared to 42 for Hispanic residents and 17 for Black residents.
A lack of confidence in navigating the health system is one contributing factor; others are a relative dearth of community-based health care options in economically disadvantaged areas, as well as transportation costs connected to getting to and from health care hubs.
While health disparities often are framed through a race- or gender-based lens, “a lot of these health-related social needs are really rooted in income,” notes Rani Williams, chief diversity and community health equity officer at UI Health.
Making it easier to be healthy
Photo: Anthony Jackson

For all the complex factors that influence health outcomes — from genetics to behaviors, cultural factors, life experiences and medicine — a nutritious diet is among the most important. For health professionals, encouraging people to eat healthfully means making it easy to cook and eat well.
So when Chef Polk leads the South Shore cooking classes, he recommends widely available ingredients that participants can get without traveling too far. Lofton, the UIC researcher behind the program, is mindful of participants who rely on public transportation or ride-shares to get to stores that, in disadvantaged areas, are often located far from home.
For people who don’t have access to nearby parks or who don’t feel safe outdoors, another staple of preventive health care — exercise — can be similarly challenging.
Those are the situations that get high-level systems designers such as the Institute for Healthcare Delivery and Design’s Musick to think about community- or policy-level interventions, while on-the-ground practitioners such as Silvia Lara from the Davis Health and Wellness Center focus on devising workarounds such as YouTube workouts and at-home push-up regimens.
Yet beyond administering care and sharing best practices, among the most powerful gifts a provider can offer to a patient are hope and confidence.
These days, cooking-class participant Katrina Gatson is feeling both as she’s grown passionate about cooking healthfully for herself and her family.
She’s got a piece of advice for would-be chefs that could also serve as a prescription for a country and health system looking to improve the care it delivers: “Try new things,” Gatson says. “Don’t be afraid. Just because you tried something one way doesn’t mean you couldn’t try it a different way and like it even better.”