By Anthony Jackson
From Addiction to Advocacy
How UIC’s Community Outreach Intervention Projects employs local leaders for street outreach, health care services, needle exchange and more for people who use drugs.
When it comes to working with her clients, Nieves relates to them through her own experiences with addiction.
“They have told me, ‘I like talking to you because you’ve been there. You’re not the person who knows it through books and stuff,’” Nieves said. “They like talking to people who have used and are clean; it gives them a little pep, like ‘If she did it, then I can do it.’”
COIP employs people who are in recovery from using drugs to help deliver services and assist in research. Known as their Indigenous Leader Outreach Model, the program reduces barriers to health care for clients, such as the stigma associated with substance use, to help establish relationships and build trust among people who inject drugs and other underserved populations.
These outreach leaders have assisted with research topics studying interventions to prevent hepatitis C and HIV among young drug users, mental health’s impact on HIV risk behaviors, transitions from heroin snorting to injection, effectiveness of needle exchange programs and more.

Maria Nieves poses for a portrait in her office at COIP's Austin location. Photo: Anthony Jackson
Maria Nieves is never alone. She always has another person with her – a colorful tattoo of a young woman on her forearm, which covers track marks from when she used to inject heroin.
Nieves beat her addiction in 1996, and two years later she started volunteering with the University of Illinois Chicago School of Public Health’s Community Outreach Intervention Projects (COIP).
Now, 25 years on, Nieves is a full-time field site supervisor at COIP’s Austin location. She works with people who inject drugs, oversees needle exchanges and manages HIV and hepatitis testing, among other services.
That same year, the Cook County Medical Examiner’s Office recorded more than 1,500 opioid overdose deaths; of those, 90% involved fentanyl.
In 2023, COIP’s Austin location exchanged almost 23,000 needles.
For almost 40 years, COIP’s needle exchange program in Chicago’s Austin neighborhood has helped reduce the chances of people sharing contaminated needles and ensured their proper disposal.
Photo: Anthony Jackson


COIP's harm reduction services educate people who use not only opioids but other street drugs like crack cocaine, pharmaceutical pills and meth, as well as those who use drugs by means other than injection, to prevent illnesses and fatalities that can arise from using drugs.
COIP’s Austin location is situated among three of Chicago’s highest-impacted communities for opioid-related deaths: Austin, West Garfield Park and Humboldt Park, according to a 2021 Midyear Opioid Report from the Chicago Department of Health.

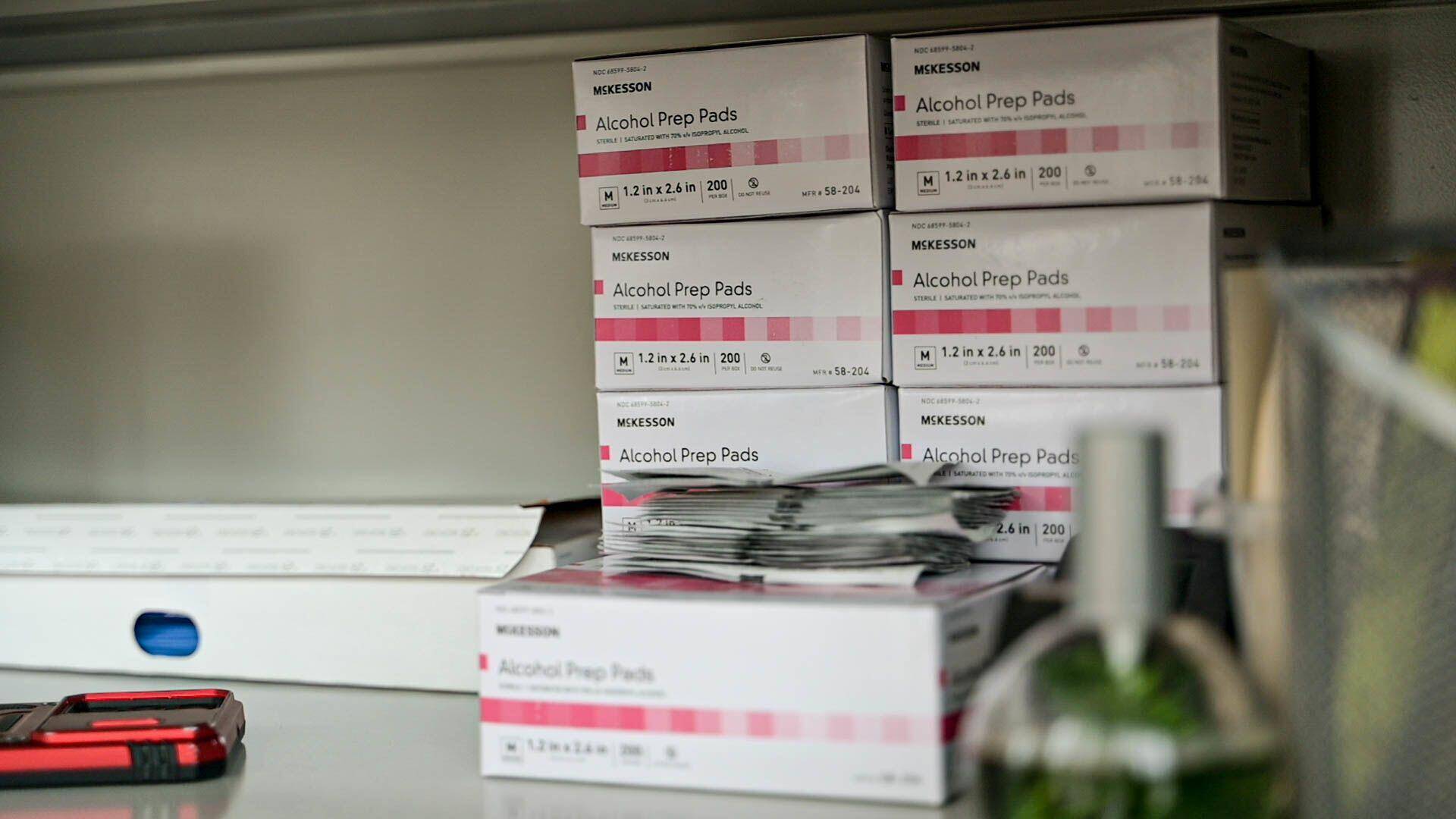
COIP's social services range from providing bus passes, helping clients prepare important documents, clothes donations and more. Photo: Anthony Jackson
Expanding Care
At its founding in 1986, COIP offered testing, case management and support for people who injected drugs to address the HIV/AIDS crisis.
Its operations have significantly expanded over the past 38 years to include street outreach, overdose education, risk reduction, recovery support and counseling as part of COIP’s “full circle of care,” according to COIP Services Director Maria Nava BA ’98, MPA ’13.
“The focus of the program started in harm reduction but has branched out into different services,” Nava said. “Because you can’t just provide the harm reduction services without providing social services.”
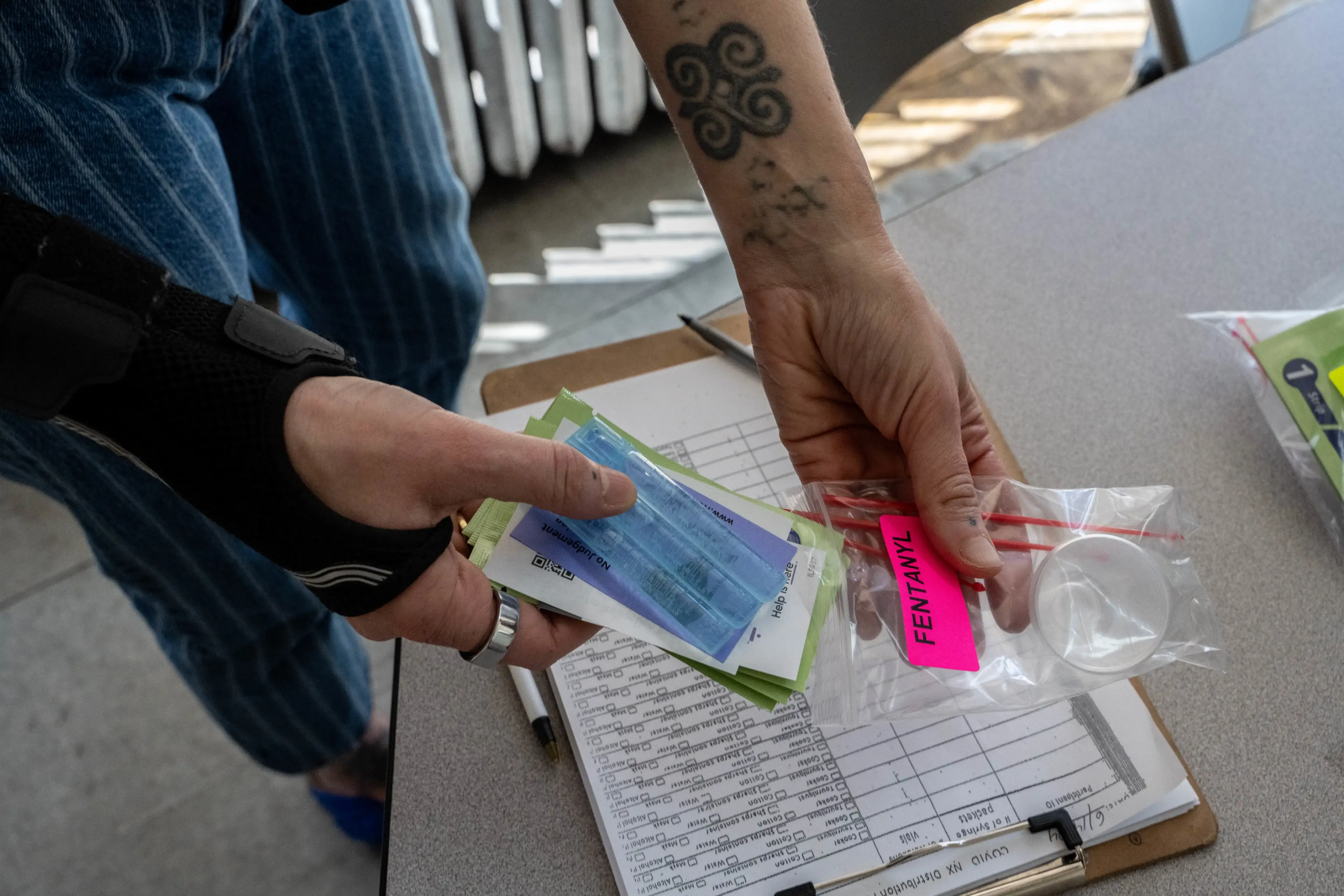
COIP provides clients with self-administered tests, such as this one for fentanyl.
COIP’s sample collection box allows clients to test drugs for impurities, which can be fatal.
Photo: Anthony Jackson
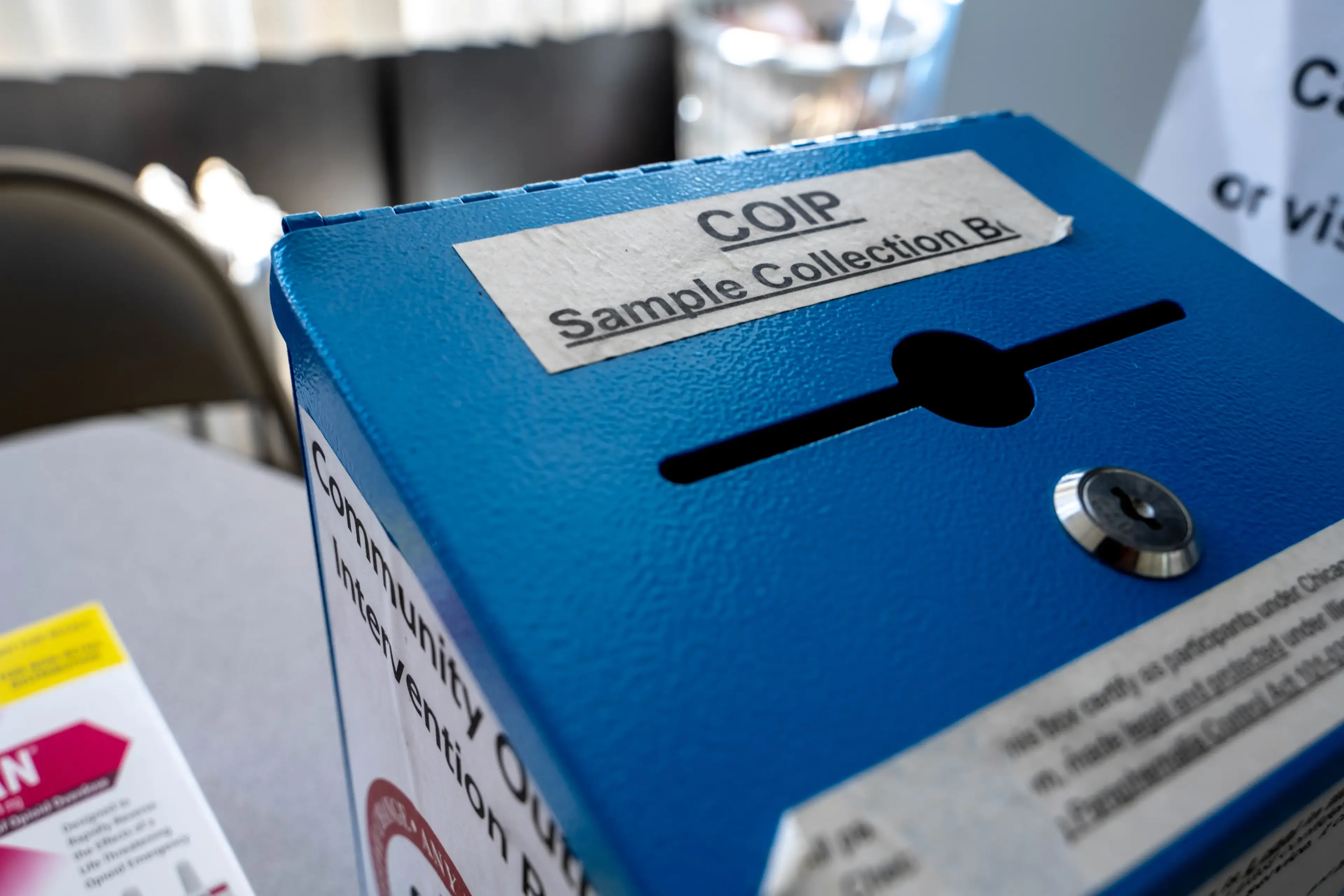
COIP’s sample collection box allows clients to test drugs for impurities, which can be fatal.
Photo: Anthony Jackson

and another is supplied with clothing and food donations.
One holds harm-reduction supplies, another has a private doctor’s office with a shower and bathroom,
Each van houses a critical piece of health care infrastructure.
Photo: Anthony Jackson
“Working with this population is very unpredictable, but either way, we’re prepared to provide services when they need it,” COIP Clinical Services Coordinator Albert Murphy BA ’15, MPH ’20 said.
Brian Schoneck has been with COIP for nearly two years. He is turning his experience recovering from addiction into a career as a substance abuse counselor and is working to be a certified counselor for alcohol and other drugs.
Outreach leaders see the positive effects of the program. However, when coupled with housing, food insecurity and poverty, addiction becomes harder to overcome.
“What we try to do is navigate around all those other issues and variables that people face. It is a big help to the community, but it needs to be bigger,” said Ernest Mosby, a COIP outreach leader. “More of the community needs to get involved.”
As COIP expands its services, program leaders hope to create space and funding to provide safe injection sites for clients through policy advocacy.
“I think a safe injection site will help people who are not ready for treatment but could use a safe space and somebody that monitors them to make sure they don’t overdose,” Murphy said. “And then there’s all these other services there for when they are ready.”

COIP Clinical Services Coordinator Albert Murphy BA ’15, MPH ’20 looks through a box of drug tests in one of COIP's mobile units. Photo: Anthony Jackson
Health Care On Wheels
On a Friday this June, a trio of vans parked at the corner of Homan and Chicago avenues in Humboldt Park, along the edge of an empty dirt lot where a store once stood.
From there, they traveled to Douglass Park on Chicago’s southwest side. A few days prior, COIP leaders learned through word-of-mouth that there were multiple overdoses at this location. Outreach leaders canvassed the park but found it empty.
One-by-one, outreach leaders make connections and increase COIP’s visibility, hoping they will see them again.
Because of COIP’s mobile operations, community outreach leaders can increase efforts in understanding community needs and providing help and resources for people who are addicted to drugs.
Photo: Anthony Jackson



By Anthony Jackson
From Addiction to Advocacy
How UIC’s Community Outreach Intervention Projects employs local leaders for street outreach, health care services, needle exchange and more for people who use drugs.
When it comes to working with her clients, Nieves relates to them through her own experiences with addiction.
“They have told me, ‘I like talking to you because you’ve been there. You’re not the person who knows it through books and stuff,’” Nieves said. “They like talking to people who have used and are clean; it gives them a little pep, like ‘If she did it, then I can do it.’”
COIP employs people who are in recovery from using drugs to help deliver services and assist in research. Known as their Indigenous Leader Outreach Model, the program reduces barriers to health care for clients, such as the stigma associated with substance use, to help establish relationships and build trust among people who inject drugs and other underserved populations.
These outreach leaders have assisted with research topics studying interventions to prevent hepatitis C and HIV among young drug users, mental health’s impact on HIV risk behaviors, transitions from heroin snorting to injection, effectiveness of needle exchange programs and more.

Maria Nieves poses for a portrait in her office at COIP's Austin location. Photo: Anthony Jackson
Maria Nieves is never alone. She always has another person with her – a colorful tattoo of a young woman on her forearm, which covers track marks from when she used to inject heroin.
Nieves beat her addiction in 1996, and two years later she started volunteering with the University of Illinois Chicago School of Public Health’s Community Outreach Intervention Projects (COIP).
Now, 25 years on, Nieves is a full-time field site supervisor at COIP’s Austin location. She works with people who inject drugs, oversees needle exchanges and manages HIV and hepatitis testing, among other services.
That same year, the Cook County Medical Examiner’s Office recorded more than 1,500 opioid overdose deaths; of those, 90% involved fentanyl.
In 2023, COIP’s Austin location exchanged almost 23,000 needles.
For almost 40 years, COIP’s needle exchange program in Chicago’s Austin neighborhood has helped reduce the chances of people sharing contaminated needles and ensured their proper disposal.
Photo: Anthony Jackson

COIP's harm reduction services educate people who use not only opioids but other street drugs like crack cocaine, pharmaceutical pills and meth, as well as those who use drugs by means other than injection, to prevent illnesses and fatalities that can arise from using drugs.
COIP’s Austin location is situated among three of Chicago’s highest-impacted communities for opioid-related deaths: Austin, West Garfield Park and Humboldt Park, according to a 2021 Midyear Opioid Report from the Chicago Department of Health.

COIP's social services range from providing bus passes, helping clients prepare important documents, clothes donations and more. Photo: Anthony Jackson
At its founding in 1986, COIP offered testing, case management and support for people who injected drugs to address the HIV/AIDS crisis.
Its operations have significantly expanded over the past 38 years to include street outreach, overdose education, risk reduction, recovery support and counseling as part of COIP’s “full circle of care,” according to COIP Services Director Maria Nava BA ’98, MPA ’13.
“The focus of the program started in harm reduction but has branched out into different services,” Nava said. “Because you can’t just provide the harm reduction services without providing social services.”
Expanding Care
Photo: Anthony Jackson
COIP provides clients with self-administered tests, such as this one for fentanyl.
COIP’s sample collection box allows clients to test drugs for impurities, which can be fatal.
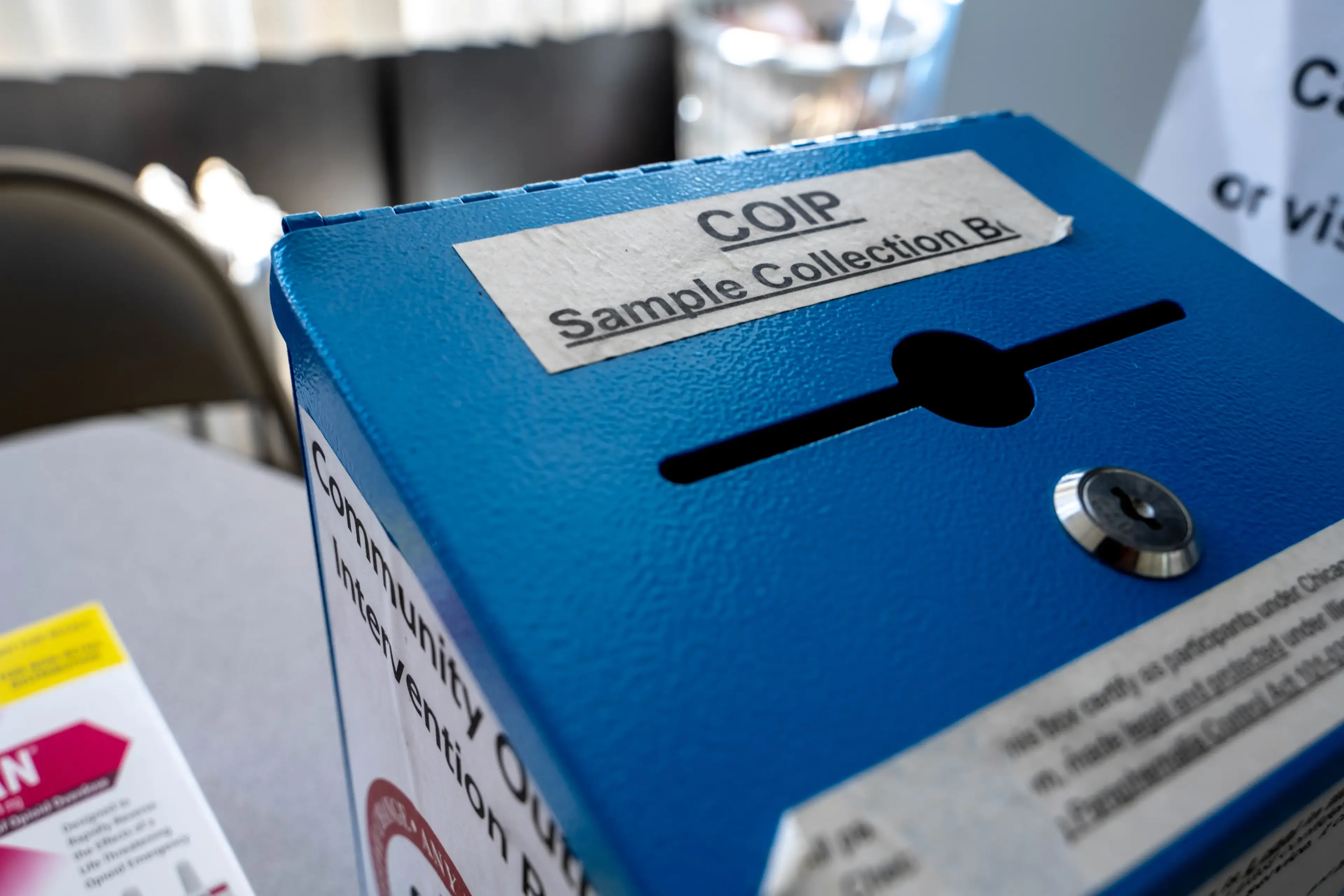
COIP’s sample collection box allows clients to test drugs for impurities, which can be fatal.
Photo: Anthony Jackson
and another is supplied with clothing and food donations.
One holds harm-reduction supplies, another has a private doctor’s office with a shower and bathroom,
Each van houses a critical piece of health care infrastructure.
Photo: Anthony Jackson
“Working with this population is very unpredictable, but either way, we’re prepared to provide services when they need it,” COIP Clinical Services Coordinator Albert Murphy BA ’15, MPH ’20 said.
Brian Schoneck has been with COIP for nearly two years. He is turning his experience recovering from addiction into a career as a substance abuse counselor and is working to be a certified counselor for alcohol and other drugs.
Outreach leaders see the positive effects of the program. However, when coupled with housing, food insecurity and poverty, addiction becomes harder to overcome.
“What we try to do is navigate around all those other issues and variables that people face. It is a big help to the community, but it needs to be bigger,” said Ernest Mosby, a COIP outreach leader. “More of the community needs to get involved.”
As COIP expands its services, program leaders hope to create space and funding to provide safe injection sites for clients through policy advocacy.
“I think a safe injection site will help people who are not ready for treatment but could use a safe space and somebody that monitors them to make sure they don’t overdose,” Murphy said. “And then there’s all these other services there for when they are ready.”

COIP Clinical Services Coordinator Albert Murphy BA ’15, MPH ’20 looks through a box of drug tests in one of COIP's mobile units. Photo: Anthony Jackson
On a Friday this June, a trio of vans parked at the corner of Homan and Chicago avenues in Humboldt Park, along the edge of an empty dirt lot where a store once stood.
From there, they traveled to Douglass Park on Chicago’s southwest side. A few days prior, COIP leaders learned through word-of-mouth that there were multiple overdoses at this location. Outreach leaders canvassed the park but found it empty.
Health Care On Wheels
One-by-one, outreach leaders make connections and increase COIP’s visibility, hoping they will see them again.
Because of COIP’s mobile operations, community outreach leaders can increase efforts in understanding community needs and providing help and resources for people who are addicted to drugs.
Photo: Anthony Jackson